Category: OB
IV Fentanyl while waiting for labor epidural
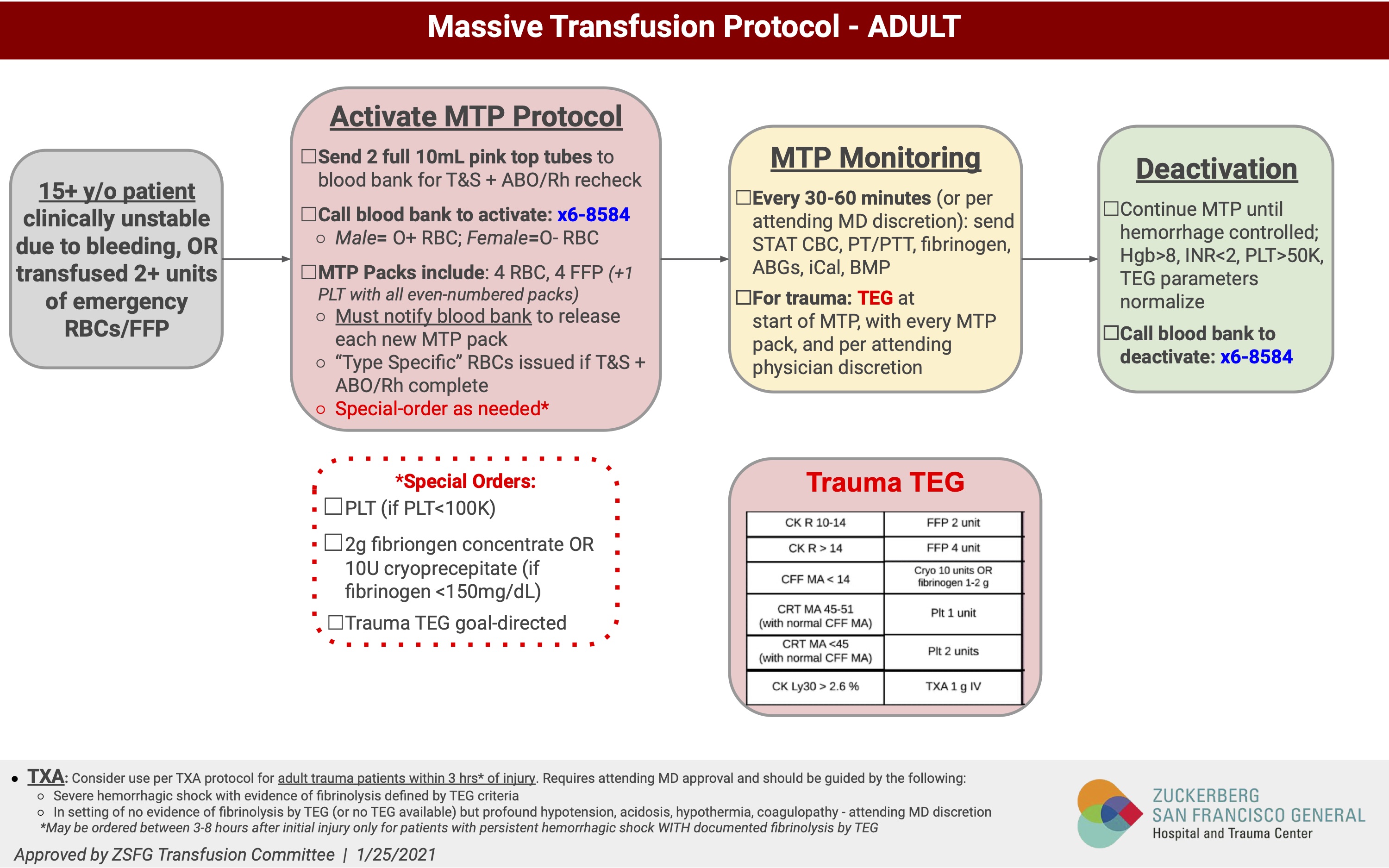
Massive Transfusion Protocol
Basics: Blood Transfusion, StatPearls
Massive transfusion: a review. Vol 7 (June 30, 2022).
One means of achieving a balanced resuscitation is with the use of WB instead of component therapy. The combination of plasma, PLT and PRBC components in a 1:1:1 ratio is estimated to result in a HCT of 25%, coagulation factor activity of 62%, platelet concentration of 50×109/L, and fibrinogen concentration of 75 mg/dL. In comparison, a unit of fresh WB has a HCT of 45%, 100% activity of all coagulation factors, platelet concentration of 200×109/L, and fibrinogen concentration of 150 mg/dL
Massive transfusion: a review. Vol 7 (June 30, 2022).
OB Hemorrhage
The American College of Obstetricians and Gynecologists (ACOG) recommends fixed product ratios (65). This practice is supported by retrospective studies that demonstrate, in combination with a comprehensive post-partum hemorrhage protocol, MTP is associated with improvement in transfusion needs and peri-partum hysterectomy (66–68). Additionally, obstetric hemorrhage protocols should focus on repletion of fibrinogen via early administration of CRYO or fibrinogen concentrate, as fibrinogen is the first coagulation factor to diminish in post-partum hemorrhage
Massive transfusion: a review. Vol 7 (June 30, 2022).
Adjuncts to MTP
In addition to blood transfusion during MTP, several useful pharmacologic adjuncts to resuscitation have been identified. These include calcium repletion, tranexamic acid (TXA), factor VII concentrate, prothrombin complex concentrate (PCC), and arginine vasopressin (AVP). In addition to pharmacologic adjuncts, the use of viscoelastic testing can help improve blood product utilization and outcomes.
Massive transfusion: a review. Vol 7 (June 30, 2022).
Adverse Effects of MTP
One in 455 blood components transfused is associated with an adverse event, but the risk of serious adverse reactions (1 in 6,224) and transfusion-transmitted infections (1 in 255,400) is extremely low in the United States (117). The most common non-infectious reactions include febrile non-hemolytic transfusion reactions, allergic transfusion reactions, transfusion-associated circulatory overload (TACO), transfusion-related acute lung injury (TRALI), and acute or delayed hemolytic reactions (118). The effects of blood preservation and storage also cause changes in the quality of the blood over time, including decreased pH, increased potassium, decreased 2,3-diphosphoglycerate (2,3-DPG), and decreases in erythrocyte and platelet function, all of which may affect resuscitation and oxygen delivery (119).
Massive transfusion: a review. Vol 7 (June 30, 2022).
Internet Book of Critical Care: Massive Transfusion Protocol



Trigger for FFP and/or PCC in Clinical Recommendations
In the Society of Cardiac Anesthesiology recommendations, transfusion of 10 to 15 ml/kg of FFP or a low dose of PCC (not defined) is recommended when clotting time in tissue factor–activated ROTEM or the reaction time in heparinase TEG is significantly prolonged (table 2).13 Of note, the European recommendations for hemostatic resuscitation in trauma recommend a dose of 25 IU/kg of a PCC, whereas in cardiac surgery patients, an initial dose of 12.5 IU/kg (similar to that suggested by the U.S. recommendations) should be considered because of the inherent risk of thromboembolism.20 In the European trauma guidelines, the authors point out the possible influence of hypofibrinogenemia on clotting time in tissue factor–activated ROTEM.14 Therefore, PCC should be given only when fibrinogen levels are less than 1.5 g/l (corresponding to a fibrinogen ROTEM maximal clot firmness of less than 10 mm), and clotting time in tissue factor–activated ROTEM is prolonged or remains prolonged after replacement of fibrinogen.
Viscoelastic Coagulation Testing: Use and Current Limitations in Perioperative Decision-making. Anesthesiology August 2021, Vol. 135, 342–349.

Trauma Quality Improvement Program: MTP in Traumas
Massive Transfusion Protocol In: LITFL – Life in the FastLane, Accessed on April 20, 2023.
Canadian Blood Services: Massive hemorrhage and emergency transfusion
Massive Transfusion Protocol Template
UCSF Massive Transfusion Protocol
Washington State: Massive Transfusion Protocol


Red Cross: Transfusion Guidelines


WB RECOMMENDATIONS
Whole Blood Transfusion, Military Medicine, Volume 183, Issue suppl_2, September-October 2018, Pages 44–51.
- − SWB, which will in U.S. military practice be LTOWB, is the preferred product for resuscitation of severe bleeding (both pre-hospital and in-hospital). SWB simplifies the logistics of the transfusion and may facilitate more rapid resuscitation of casualties, and may enhance a facility’s capacity to manage mass casualty (MASCAL) challenges.
- − The indication for SWB is life-threatening hemorrhage. The assessment that a hemorrhage is life-threatening is mainly established clinically, and should be driven by an assessment of the patient’s vital signs, hemodynamics, physical exam, mechanism of injury and laboratory measures of shock and hemostasis if available. The use of FWB should be reserved for when SWB or full component therapy is unavailable.
- − Blood component therapy (1:1:1) is an acceptable option for treating life-threatening hemorrhage when SWB is not available. The potential reduced efficacy, safety, and logistical aspects of blood component therapy should be taken into consideration when choosing between resuscitation strategies (Table I).

Intraperitoneal Chloroprocaine
20-something year old primip came today with preeclampsia and was deemed a c/s candidate for her 26 week baby. She was 5’8″, 165lb and had no prior issue with previous surgeries. She was started on magnesium preop. The mag was held intraoperatively and would resume postoperatively. Pt was in sitting position for her spinal, which was placed at L4-5. Good clear CSF return. 0.75% bupi dosed at 13.5 mg with intrathecal fentanyl 15mcg and intrathecal morphine 0.2mg. BP decreased from 150s to 130s, which was appropriate. Patient stated she had increased tingling and decreased mobility in her legs. All symptoms and signs appropriate with her spinal. Patient passed the Allis clamp test prior to incision. She was quite anxious: propofol was given IV for anxiolysis. Patient was adamant about breastfeeding/pumping for her baby. No complications with delivery. Uterus was externalized and patient was sensitive to pressure and tugging/manipulation. IV fenatnyl and IV morphine were given along with IV propofol. When uterus was internalized, patient felt more pressure that seemed unbearable. More IV pain meds were given. Suggestion was made for intraperitoneal chloroprocaine. Patient able to tolerate fascial closure as well as staple skin closure.
Intraperitoneal chloroprocaine
Pain Control During Cesarean Delivery. Anesthesia Experts. Jan 2020.
Failed epidural
Doctoring and Mothering Today
Now that my oldest is almost 4 years old and my youngest is almost 3… it’s a good time to reflect back on my time during pregnancy, post-partum, breastfeeding, maternal/family leave, full-time work, and raising 2 toddlers.
Pregnancy:
Pregnancy really was a wonderful time. Aside from the GERD, waddles, having to pee all the time and drinking a ton of water… it was wonderful feeling the little kicks and getting the attention of people to always help me (open a door, lift things, walk with me, etc.). I worked up until I went into labor… literally.


The most difficult things to do during MY pregnancy: make appointments, drink enough water, peeing every 2 hours (even during the night), eating (I could only take 4-5 bites before getting full), sleep.
Post-Partum
No one tells you what to expect post-partum. It’s a rude awakening when it’s really difficult to have a BM, wipe, breastfeed, wake up, and think clearly. For me, the SI joint pain from pregnancy lingered on even until today. Bonding with baby is unique and special. It was a wonderful time to watch my babies explore their senses. Sleep and breastfeeding: It’s really tough to get in enough sleep and breastfeed constantly. But after 2 weeks, breastfeeding got better for me. Maybe I was lucky. Sleep got better for me after 2 months After the 2nd kiddo, I think I had a bit of postpartum depression. Coupling the lack of sleep while also trying to be present for a 13-month old really wore me down. I was in a really dark place: the thoughts, the lack of care of harm to myself, the total loss of happiness for things I previously enjoyed. It was all very real, very memorable, and something that I look back on with sadness bc I wasn’t my best for the kids, my hubs, or myself. I’m thankful to have moved beyond that. The Peloton saved me on this one. I told NO ONE.
Breastfeeding:
Rent a hospital-grade breast pump prior to leaving the hospital. Visit with the lactation consultant while at the hospital to really learn how everything works. I was lucky to have a great LC for both deliveries. The first one really encouraged me and taught me good technique. The second was fabulous as she supported me and encouraged my efforts while also allowing me to opt for normalcy and not beat myself up if my milk production wasn’t 100%. Both excellent teachers and perspectives. Breastfeeding is new and it’s hard. Get help early and often! When you come back to work, do what you can. I oftentimes pumped in the OR and immediately put my stash in the freezer during breaks. This became really tough for me as breaks are uncertain and you don’t want to burden people who also need breaks. My milk supply went down fast, but I did what I could and that was my best. Don’t beat yourself up.
Maternal/Family Leave:
I was really lucky to be able to have 3 months off work. My anesthesia group was absolutely wonderful in allowing bonding time. I took the full 3 months. My husband then took his 1 month and we were able to do a solid bond with the kiddos for 4 months and then put them into daycare when they were 5 months old. Would it be great if we had full pay for 1 year of maternal/family leave? Yes. But, in the US, this is the best I could get and I’m grateful for it!
Full-time Work:
This was my own decision to continue working full-time. You can see in the charts above. After my second baby, I came back and still worked full-time. This was a personal choice. Kids are innocently demanding…. so is my job. I don’t really know how to find that right balance just yet. I miss out on my babies, and I miss out on work. In the end, you have to be ok with not being the best at everything. You will make sacrifices and you will feel awful. It was be a gut punch that you readied yourself for, but still feel every ounce of hurt when you miss things. The first tuck-in, the first goodnight kiss, the many goodbyes, the bathtime shenanigans, the sweet baby smells…. you will miss them. It gets easier. But, it still hurts when you miss these things. It’s almost like life moves on without you. That is…. until you get back and see the smiles and feel the hugs and kisses from them.
Raising 2 toddlers 13 months apart:
This is something! We brought home our second baby just after our 1st baby turned a year old. I don’t think the concept of a sibling coming to the house was even a concept that a one year old can grasp. Having two kids so close in age, but at different stages of development was REALLY HARD. They are just now starting to play together and sharing appropriately. It is still hard for us despite both kiddos being potty-trained (nighttime diapers only for my sanity). Everyone says 5 years old is the magical age where things get easier. We’re almost there!
During the delivery of our 2nd kiddos, I had a moment of weakness and thought a third child would be great. The second delivery was significantly easier than the first. Perhaps my body and mind were playing tricks on me. We feel complete. We have two beautiful and healthy kids. We couldn’t ask for more.
Mothers in Medicine: Making Residency Safer in Pregnancy
A Penned Point: Give yourself a break–Don’t have a baby during residency. March 2012.
Responsibility for your own health
I was shocked to see that the NHS could ban surgery for the obese and smokers. That’s socialized medicine. You take a conglomerate group of people (the UK) on a limited budget for healthcare… and basically find the cheapest most cost-effective way to deliver healthcare. But in a way, it’s empowering patients to take responsibility for their own health. Smoking, for sure — I agree 100% that surgery should be banned for this population. Obesity is a bit trickier — there’s genetics and environmental factors at play in this one. I don’t think anyone chooses to be obese. But, people do have the power to change their eating and exercise habits. Despite these efforts, there are some people who are still obese…. and these people should not be faulted.
Why single out the obese and smokers?
Smokers and the obese have elevated surgical risk and mortality, which means more cost to treat and hospitalize and provide ongoing care.
I think the NHS is on to something here. They’re opening doors to moving the liability and responsibility away from physicians and towards patients. This is a plus. Outsiders may see it as separatism and elitist to only provide care for people who are healthy. But look at the facts and the data…. obesity has a lot of co-morbidities associated. Smoking has a lot of co-morbidities associated as well. Why should physicians be penalized for re-admissions, poor wound healing, longer hospitalizations when the underlying conditions themselves are already challenging enough? In fact, I would urge insurance companies to provide incentives to patients/the insured with discounted rates for good and maintained health and wellness. With all the technologies, medications, and information out there, it’s time patients take responsibility for their own health. I take responsibility for mine — watching my diet, exercising, working on getting enough rest, maintaining activities to keep my mind and body engaged, meditating for rest and relaxation. It’s not easy, but my health is 100% my responsibility. I refuse to pass the buck to my husband, my family, my physician, etc. I do what I can to optimize my health and future — and if that doesn’t work… I call for backup.
Patients need to change their mindset re: health. It is not your spouse’s responsibility to track your meds. It is your responsibility to know your medical conditions and surgical history. The single most important (and thoughtful) thing a patient can do is keep an up-to-date list of medications, past/current medical history, surgical history, and allergies to bring to every doctor’s appointment and surgery. This helps streamline and bring to the forefront your conditions and how these will interplay with your medical and surgical plan and postoperative care. Please do not forget recreational drugs, smoking habit, and drinking habit in this list. It is very important to know all of these things. Also, your emotional history is very important. Depression, anxiety, failure to cope, etc. This all helps tie in your current living situation with stressors and your medical history.
Links for educating yourself in taking responsibility for your health:
- Patients Should Share Accountability for Own Health — A new report recommends doctors not be penalized for poor outcomes if patients fail to follow recommended protocols
- Getting patients to take responsibility for their own health
-
Responsibility for health: personal, social, and environmental
- Responsibility, fairness and rationing in health care.
- What the Health documentary
Emergency Checklists
It seems like in today’s day and age, emergencies are occurring everywhere. From hurricanes to shooters to earthquakes and fires… I think it’s always important to know what to do. Here are some fabulous checklists I’ve found for getting through those emergencies. These are not substitutions for knowledge and training. Clinical judgement warranted.
Emergency Manual from Stanford — Printable PDF
Ariadne Labs OR Crisis Checklist
Ariadne Labs Safe Surgery Checklist Template
Ariadne Labs Ambulatory Safe Surgery Checklist Template
Newton-Wellesley’s L&D Checklists
Checklist for Trauma Anesthesia
ASRA checklist for Local Anesthetic Systemic Toxicity
Johns Hopkins Central Line Checklist
STS Adult Cardiac Surgery Checklist
Ariadne Labs Cardiac Surgery Checklist
STS General Thoracic Surgery Checklist
STS Congenital Heart Surgery Checklist
Walking labor epidurals
- American Pregnancy Association: Epidural Anesthesia
- N Engl J Med 2010;362:1503-10. Epidural analgesia for labor and delivery.
What is a “walking” epidural?
MJAFI, Vol. 63, No. 1, 2007. Walking Epidural : An Effective Method of Labour Pain Relief.
Int J Women’s Health, 2009, 1: 139-154. Advances in labor analgesia.

Clinical Guidelines: Labour Analgesia. Jan 2017. King Edward Memorial Hospital, Australia.
Contin Educ Anaesth Crit Care Pain (2004) 4 (4): 114-117. Epidural analgesia in labor.

From the ASA 2017 (October in Boston):
-
CSE: 1 cc 0.25% bupi + 15mcg fentanyl (good for primip)
-
25g Dural Puncture without dosing sometimes (primips)
My other OB blog links:
2015 in review
The WordPress.com stats helper monkeys prepared a 2015 annual report for this blog.
Here’s an excerpt:
A San Francisco cable car holds 60 people. This blog was viewed about 2,000 times in 2015. If it were a cable car, it would take about 33 trips to carry that many people.
OB Anesthesia
Today, I’m on call covering OB.

MGH: OB anesthesia Q&A for patients
BWH: OB anesthesia Q&A for patients
IARS 2010: OB anesthesia in the 21st century
IARS 2011: OB anesthesia update
Indian J Anesthesia 2006: Acute Pain – Labour Analgesia
Presentation on mobile epidural
June 2011: Update on rural OB anesthesia
Oct 2013: Presentation on Labor analgesia. Epidural vs CSE, bolus v infusions

To epidural or not to epidural. That is the question.
A great YouTube video on what an epidural is and what it will feel like.
YouTube vid of a real epidural placement ** Needles are involved in this one**
Lately, I’ve been changing my regimen for pain control with PCEA. It seems most of my partners use a 10ml/hr basal rate, 5ml bolus dose, 10 minute lockout, and 30 ml/hr max.
My current strategy for PCEA (0.0625% bupi + 2mcg/ml fentanyl):
- 5ml/hr basal rate
- 10ml bolus
- 20 minute lockout
- 35 ml/hr max
ASA Nov 2001: PCEA during labor
Br J Anaesth 2010:Labour analgesia and obstetric outcomes.

Neuraxial anesthesia in the non-pregnant patient
Anesthesiology Research and Practice 2012: Recent advances in epidural analgesia.
Br J Anaesth 2012: Failed epidural: causes and management.
From my blog:












