I was asked to consult on a 30-something year old patient who had a recent subdural hemorrhage. It was a spontaneous event without trauma. After a week of stabilization of the SDH, the patient started developing positional headaches. CT scan showed a CSF leak from C4-T5 ventrally and another one from T6-T10 dorsally.
CT head: Small evolving right greater than left bilateral subdural hematomas, not significantly changed compared to prior. No evidence of new hemorrhage. Trace right to left midline shift is unchanged.
Cspine/T-spine/L-spine with contrast: Extensive CSF leak. The dominant component of this process is a ventral epidural contrast collection extending from C6-T4 levels, but there is also abnormal dorsal epidural contrast extending from T5-T10. The contrast is densest in the cervicothoracic ventral epidural space, also suggesting that this is the primary leakage site.
MRA neck without acute abnormalities. MRI cervical/thoracic/lumbar spine which incidentally revealed multifocal demyelinating lesions in the cervical cord with a focal lesion at T7 and MRI brain showed multiple foci of T2 flair hyperintensity in the supratentorial white matter of the brain, suspicious for undiagnosed demyelinating disease.
What is an epidural blood patch?
Recent update on epidural blood patch: Review. Anesth Pain Med 2022;17:12-23.
Typically, anesthesia gets consulted for lumbar epidural blood patches after lumbar CSF leaks. However, in this case, the CSF leak occurs quite high in the cervicothoracic spine. Oftentimes, it’s very difficult to inject a greater volume of blood in the lumbar epidural space due to back pain to reach the higher cervical and thoracic areas.

Why not do a lumbar epidural blood patch to reach the cervical or thoracic space?
One question that is often asked is whether CEBPs are necessary, or would lumbar EBPs suffice, even for dural leaks at the cervical levels. There are several reports indicating that lumbar EBP can permanently alleviate the headache regardless of whether or not the site of leakage is identified . However, other reports demonstrate that lumbar EBP does not always result in permanent relief [36–38]. A study by Diaz suggests that the site of leakage should be identified by radioisotope cisternography and treated with EBP targeted to CSF leak site levels . Cousins et al suggested that placement of the EBP close to the site of CSF leakage is important . Studies have shown that blood injected at the lumbar level does reach the cervical levels. Ferrante et al., for instance, performed epidural blood patch at L3-4 and placed in the patient in trendelenburg for 22 hours . He was able to show presence of blood in the epidural space at the cervical levels on postprocedure MRIs. The mean spread of the blood patch in the epidural space has been found to be 4.6 ± 0.9 vertebral levels . Most of the blood spread in the cephalad direction . However, the amount of blood that reaches the higher cervical levels in comparison to the amount of blood needed to form a stable clot is unclear. Despite spread of blood to cervical levels, Beards did note that after an epidural blood patch, the majority of the clot and mass effect appears to be concentrated in the area around the injection site .
Cervical epidural blood patch—A literature review. Pain Medicine, Volume 16, Issue 10, October 2015, Pages 1897–1904.

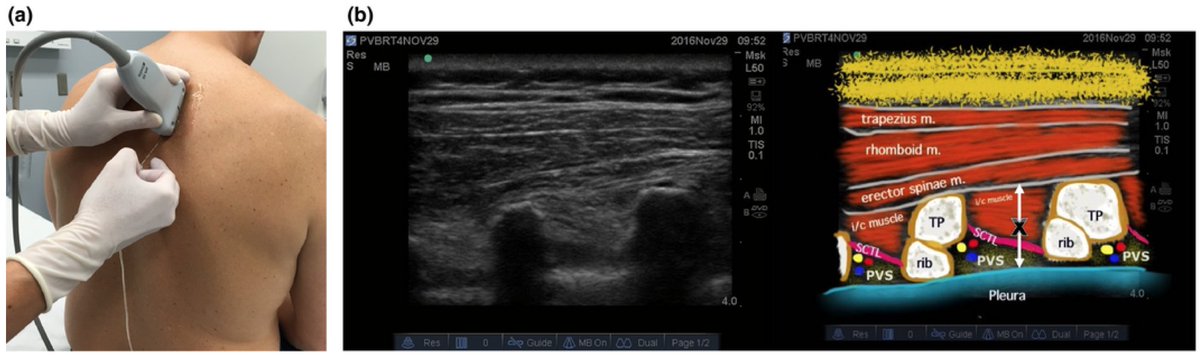
How does one reach a cervical or thoracic epidural space?

Utilizing this information, I thought this patient would be better suited for a CT-guided targeted (cervicothoracic) ventral epidural blood patch performed by the IR team. Additionally, I recommended conservative therapy: hydration, caffeine, Fioricet, lying flat, and an abdominal binder.